Prurigo Pigmentosa (PP) is a skin rash that can establish itself when people transition to a ketogenic diet. If you want to know how it looks like then you’ll find plenty of examples on Google.
On our Reddit channel r/ketoscience we have published case reports and sometimes get people questioning about it.
Obviously people who are affected by PP want to know what to do about it but also want to know what causes it.
In the following article where a dermatologist describes some background, the link with ketosis is very strong. Various cases that all lead to higher ketone production are affected by PP. There is some thought that there is inflammation triggered.
Update: 2022-01-24
A recent case published shows treatment involved cessation of the ketogenic diet and treatment with tetracyline, an antibiotic. It is effective against the Streptomyces family.
“Prurigo Pigmentosa: A Report of Two Patients in Possible Association with Essential Fatty Acid Deficiency Prurigo” https://www.turkiyeklinikleri.com/article/en-prurigo-pigmentosa-a-report-of-two-patients-in-possible-association-with-essential-fatty-acid-deficiency-prurigo-89861.html
/update
Update: 2022-10-10
PP got resolved with the antibiotic doxycycline.
“Complete remission of prurigo pigmentosa after oral doxycycline” https://onlinelibrary.wiley.com/doi/10.1111/dth.15908
/update
Update: 2023-02-01
PP got resolved through treatment with tetracycline. It is not clear if PP got resolved because of this treatment or not because the subjects were also asked to stop the ketogenic diet. It is also not clear when they were asked. Before the treatment or when they showed up after 4 weeks for follow-up by when PP already got resolved.
“A Rare Case of Prurigo Pigmentosa in a Danish Sibling Couple” https://www.karger.com/Article/FullText/528422
/update
Linking the observations
Although what I’ll show in this article is in no way proven, the links are quite strong to suspect that I’m close to the reality. Just through observation we can find the following associations
- One of the things noted is that the affected areas are often the areas where people produce more sweat. But not exclusive.
- Asians seem to be more easily affected
- Case reports reveal that anti-biotics resolve/ammeliorate PP
- Ketosis is a necessary factor
The anti-biotics is already a strong indicator that it could be bacteria related. What is unique about ketosis are the metabolites that are produced which are acetoacetate, acetone and beta-hydroxybutyrate.
Acetoacetate is further metabolized into acetone and beta-hydroxybutyrate. beta-hydroxybutyrate is confined in our blood and requires endothelial transfer via specific transporters. This doesn’t coincide well with the affected areas in the skin as they are regional.
So acetone seems to be a good candidate to look into. It is the product that is known for the ‘keto-breath’ and evaporates easily. The affected areas are often on the upper skin, from the liver upwards but that doesn’t have to mean much.
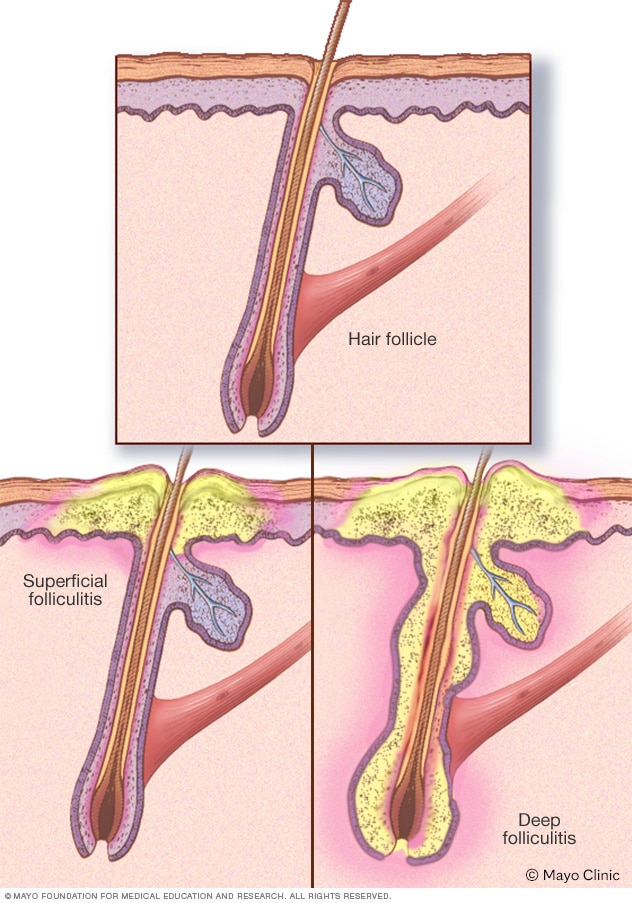
OK, let’s see if there is a connection between bacteria and acetone. The article above described an inflammatory response to bacterial folliculitis.
The histologic presence of follicular bacterial colonies supports the theory that prurigo pigmentosa may be a reactive inflammatory response to bacterial folliculitis.
Looking into bacterial folliculitis we find the bacteria Staphylococcus aureus (Sa) popping up as a resident on our skin.
Bacterial folliculitis. This common type is marked by itchy, white, pus-filled bumps. It occurs when hair follicles become infected with bacteria, usually Staphylococcus aureus (staph). Staph bacteria live on the skin all the time. But they generally cause problems only when they enter your body through a cut or other wound.
What are the effects of acetone on Sa?
With Staphylococcus aureus and Streptococcus pyogenes, acetone washed forearms had 2- to 510-fold more organisms than the control arm (P = 0.0008 and 0.08, respectively). Similar results were noted with ether (average 1:62, P = 0.005). Candida albicans increased 2- to 200-fold (average 1:37, P = 0.002). This effect did not occur with Escherichia coli and Pseudomonas aeruginosa (P = 0.8). To determine the time required for natural replenishment of the antimicrobial substances, bacteria were applied 2, 3, and 5 hours after washing with acetone.
Wow, in this experiment they used acetone to wash away the anti-microbial substances! Acetone makes these bacteria on the skin thrive.
“SURVIVAL OF PATHOGENIC MICROORGANISMS ON HUMAN SKIN” (short link)
I found a second experiment from 1965 where acetone increased bacterial count in a similar way.
“Antibacterial action of human skin. In vivo effect of acetone, alcohol and soap on behaviour of Staphylococcus aureus.” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2093882/?page=3
This establishes a clear link between acetone and bacterial growth, specifically Sa as the one that is very comfy on our skin.
What are the effects of acetone on Helicobacter pylori?
PP has also been associated with other bacteria such as Helicobacter pylori. If I’m not mistaking, normally it resides in the stomach, intestines but not in the skin. However, the presence of acetone throughout the body may enable it to migrate and survive in these places and reside in areas where acetone is more concentrated such as in the sweaty areas. It is guess work on how it gets there but it has certainly been noted that HP can be found outside the gastrointestinal tract.
Interestingly, H. pylori has also been found in several other epithelial tissues, including the eyes, ears, nose and skin that may have direct or indirect effects on host physiology and may contribute to extragastric diseases, e.g. chronic skin diseases.
…
H. pylori possesses a plethora of enzyme activities that enables for survival at low pH in the stomach that may be also important during H. pylori-based skin infection, e.g. urease that converts urea to ammonium and carbon dioxide leading to local alkalization of acid pH in the stomach (Bury-Mone et al. 2001; Cornally et al. 2008; Tuzun et al. 2010). Thus, H. pylori is able to survive outside the gastrointestinal tract and its presence in other human tissues may affect host physiology and potentially provoke extragastric disorders.
source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5350214/
First doxycycline was used but due to adverse reactions, clarithromycin was started. At the time, 2002, it was an effective antibiotic against Helicobacter pylori but the bacteria now has become more resistant to it. There was no mentioning of ketosis or the ketogenic diet.
“Prurigo Pigmentosa in Association with Helicobacter pylori Infection in a Caucasian Turkish Woman” https://www.medicaljournals.se/acta/content/abstract/10.1080/000155502320323324 (click on pdf)
H. pylori is able to carboxylase acetone and use it for survival and growth.
All three H. pylori strains that have been sequenced to date contain a potential operon whose products share homology with the subunits of acetone carboxylase (encoded by acxABC) from Xanthobacter autotrophicus strain Py2 and Rhodobacter capsulatus strain B10. Acetone carboxylase catalyzes the conversion of acetone to acetoacetate. Genes upstream of the putative acxABC operon encode enzymes that convert acetoacetate to acetoacetyl-CoA, which is metabolized further to generate two molecules of acetyl-CoA.
What the above quote tells us is that it uses acetone to generate energy by converting it to acetyl-CoA.
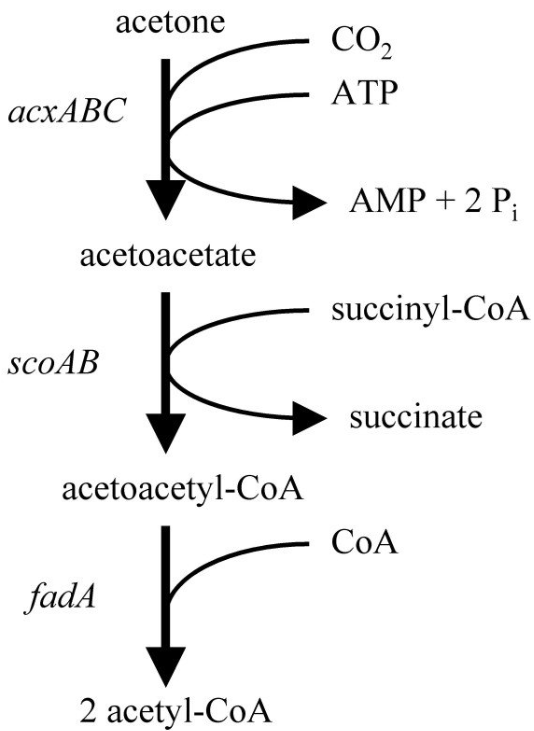
Products of the H. pylori acxABC operon may function primarily in acetone utilization or may catalyze a related reaction that is important for survival or growth in the host. H. pylori encounters significant levels of acetone in the stomach which it could use as a potential electron donor for microaerobic respiration.
“The human gastric pathogen Helicobacter pylori has a potential acetone carboxylase that enhances its ability to colonize mice” https://bmcmicrobiol.biomedcentral.com/articles/10.1186/1471-2180-8-14
What causes the damage to the skin?
The resulting thrive in H. pylori can result in a higher concentration of ammonia as the bacteria convert urea into ammonia. Strong ammonia solutions can causes serious skin burn. Possibly the chronic higher exposure (we evaporate ammonia through our skin) caused by the bacteria may equal such effect to a smaller degree.
“Regulation of Helicobacter pylori Urease and Acetone Carboxylase Genes by Nitric Oxide and the CrdRS Two-Component System” https://journals.asm.org/doi/10.1128/spectrum.04633-22
Effects of pure ammonia. I’m guessing that particularly the highlighted section in point 2 is applicable in PP:
- Dehydration. Is the result of ammonia’s great attraction for water. Anhydrous ammonia will extract water from body tissue.
- Caustic burning. Is the result of the strong base formed when ammonia combines with water from body tissue. Once ammonia extracts water from body tissue it forms ammonium hydroxide that can chemically burn tissue.
- Freezing. As liquid ammonia vaporizes it pulls heat away from body tissue causing frostbite in an instant. Released liquid anhydrous ammonia has a temperature of -28°F.
https://www.mda.state.mn.us/first-aid-information-anhydrous-ammonia-exposure
This ammonia production seems to be common in a number of bacteria as a way to survive and raise the pH level of their environment.
For some bacterial species, urease is an integral part of the bacterial acid response network, as the hydrolysis product ammonia is readily protonated into ammonium (NH4+), during which process protons are consumed, resulting in an increase in pH [1]. Urease is crucial for niche adaptation of many bacterial pathogens. For example, urease is essential for the survival of Helicobacter pylori in the stomach lining, where the pH can be as low as 2.5 [18]. With a high affinity for urea, urease from H. pylori is required not only for the establishment of infections but also for the maintenance of a chronic infection [19]. Also, Streptococcus salivarius produces urease to utilize salivary urea as a nitrogen source for growth while resisting acid stress [20]. Over 90% of S. aureus strains are urease-producing [21], which is encoded by the urease gene cluster ureABCEFGD.
“Urease is an essential component of the acid response network of Staphylococcus aureus and is required for a persistent murine kidney infection” https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1007538
This information also tells us how such infections can establish themselves. People who suffer from insufficient low stomach pH may not be killing off the bacteria sufficiently or insufficiently low stomach pH may be a sign of bacterial infection. There are other points of entry as well but whatever the cause, it would be good to look at the overall picture and see what conditions are there that allow the bacteria to enter and survive.
Acetone and the skin
Those 2 papers looking at Sa, applied acetone on the skin. Is the acetone really excreted through sweat when in ketosis? In the next paper they looked at skin acetone evaporation and found it in correlation with ketosis with emissions in the range of 0.00 to 2.70 ng/cm2/h in the studied patients. This was not on people consuming a ketogenic diet which would result in much higher levels of acetone production.
“Feasibility of skin acetone analysis in patients with cardiovascular diseases” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6141450/
Treatment
With certainty we see that anti-biotic treatment works due to the case reports. Probably not any kind of anti-biotic works, depending on the type of bacteria that is triggering the PP. Although everything seems to point to Sa, it would be a good guess to start with but until there is clear proof by sampling and analysis, we can’t say this for sure.
You could also try to treat it first through sun exposure although you may want to discuss with a dermatologist first as your skin is already inflammed. Sun exposure makes your skin produce vitamin D3. This results in the endogenously produced anti-biotic cathelicidin.
“The vitamin D–antimicrobial peptide pathway and its role in protection against infection” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2821804/
If you are afraid of the sun or have no ability to expose your affected areas to the sun then vitamin D supplementation is also effective at increasing cathelicidin. I would recommend the sun though because this provides a much higher production of vitamin D.
After supplementation with 4000 IU/d oral vitamin D for 21 days, AD lesional skin showed a statistically significant increase in cathelicidin expression from a median of 3.53 relative copy units (RCU) before supplementation to a median of 23.91 RCU postsupplementation
“Administration of oral vitamin D induces cathelicidin production in atopic individuals” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2659525/
It counteracts the biofilm that the bacteria produce to protect themselves. This biofilm has also been linked with impeded wound healing.
The helical human cathelicidin LL-37 was tested against S. aureus, and was found to exhibit effective anti-microbial, anti-attachment as well as anti-biofilm activity at concentrations in the low μg/ml range.
“LL-37-Derived Peptides Eradicate Multidrug-Resistant Staphylococcus aureus from Thermally Wounded Human Skin Equivalents” https://aac.asm.org/content/58/8/4411
“PS-302 Human Cathelicidin Antimicrobial Peptide Ll37 Influences Staphylococcus Epidermidis´ Biofilm-associated Gene-expression And Biofilm Mass On A Medical Devise Surface” https://adc.bmj.com/content/99/Suppl_2/A220.3
“Natural and synthetic cathelicidin peptides with anti-microbial and anti-biofilm activity against Staphylococcus aureus” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3397408/
I’ve already highlighted different antibiotics used in the case reports. Minocycline is another one that resolved a case of PP in 1996. No mentioning of ketosis or the ketogenic diet.
“Prurigo pigmentosa in a white woman” https://www.sciencedirect.com/science/article/abs/pii/S0190962296906313
Not any type of antibiotic resolves everything as there may be different bacterial strains at the underlaying cause. In the next case reports, 3 Italian women were treated with minocycline. This worked for 2 of them but a 3rd one did not respond. She received diaminodiphenylsulfone. It is also possible that multiple bacterial strains are at work so for clinicians I would suggest to always take a sample and check what bacteria are active.
“Prurigo pigmentosa: a misdiagnosed dermatitis in Sicily” https://pubmed.ncbi.nlm.nih.gov/10071739/
Anecdotal treatment
I’ve also scanned a few fora to see what people have tried and found helpful. They are listed here, but I would still need to find a reasonable link with either acetone or the bacteria since those 2 components are for sure involved.
- black seed oil (can also cause skin irritation)
- dandelion tea
- vitamin C (topical cream and/or oral intake)
“Anti-microbial effect of Nigella sativa seed extract against staphylococcal skin Infection” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4219874/
“Characterisation of antimicrobial extracts from dandelion root (Taraxacum officinale) using LC-SPE-NMR.” https://www.ncbi.nlm.nih.gov/pubmed/25644491
“Immunomodulatory and Antimicrobial Effects of Vitamin C” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6798581/
Vinegar can be applied to the affected skin areas but it could be wise to consult with a dermatologist to make sure there’s not more damage caused. It has anti-microbial properties and I’ve heard from one case that it helped resolve the rash. But this case drank apple cider vinegar in a diluted form multiple times a day.
Extra
As blood ketones go higher, the correlation with acetone seems to change in such a way that there is a higher increment in acetone. This study but also others I’ve seen indicate this. But the correlation doesn’t matter so much. Important to know is that as BHB goes up, so does acetone. So if you are affected, you could reduce your BHB levels while treating the bacterial issue or temporarily get off the ketogenic diet completely. You can still go low carb but just not in the ketogenic state. Although I think it is preferable to treat the bacterial problem rather than keeping them and avoiding ketosis.
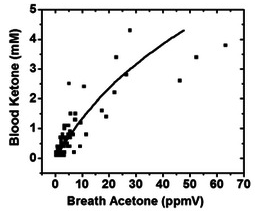
“Acetone as biomarker for ketosis buildup capability – a study in healthy individuals under combined high fat and starvation diets” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4471925/
Finally
With this piece of information I hope whoever is affected now has a good idea what to do. If all turns out to be correct then first of all you are dealing with a bacterial infection in the skin. That is priority one to resolve.
Secondly, most people are likely short in vitamin D. So get sun exposure or at least supplement after verification.
You could combine vitamin D with anti-biotic treatment to get the best result.
If all else fails then there is always the possibility to reduce the ketone production but that doesn’t help you get rid of the bacterial infection.
— THE END —
Leave a comment