Pulling the final plug on attacks
Attacks? I follow up on all published papers related to ketosis and although the execution may be done correctly and data may be generated correctly.. the circumstances are often specific and the conclusions are stretched beyond the scope of what the data is representing or can represent. All to fulfill the personal bias.
“A Short-Term Ketogenic Diet Impairs Markers of Bone Health in Response to Exercise” https://www.frontiersin.org/articles/10.3389/fendo.2019.00880/full?utm_source=F-NTF&utm_medium=EMLX&utm_campaign=PRD_FEOPS_20170000_ARTICLE
Why? The ketogenic diet is the very opposite of what is generally recommended as the ideal diet. High in (animal sourced) fat, for sure leaving out seed oils, sufficient (animal) protein and drastically limiting dietary carb intake. This goes against what nutritionists have learned and recommend and similarly for anyone in the medical field. It is also completely opposite to the ideology of other diets such as veganism.
So you can imagine it generates skepticism and enemies from different areas. Apart from clashing with personal conviction, it also threatens a whole carb-centric industry and a pharma industry that relies on managing diseases rather than handling the root cause and prevent diseases from establishing.
Since I got interested in the ketogenic diet and metabolism in general, I have found nothing left of the original negative claims and supposed dangers following a ketogenic diet (KD) except for impaired performance at very high intensities such as in endurance racing although I have a theory on how to fix that.
One last element on my list is bone health. This keeps on being a topic that comes up regularly and with this post I want to dig in deeper to understand what bone health means and what can we expect from a KD.
A first signal that made me question current dogma was when looking at pro cyclists versus amateurs. The pro cyclists had lower bone mineral density (BMD) and lower bone mineral content (BMC), both considered markers of bone health.
“Professional cyclists have lower levels of bone markers than amateurs. Is there a risk of osteoporosis in cyclist?” https://www.sciencedirect.com/science/article/abs/pii/S8756328221002672?via%3Dihub
Pro’s spend a lot more time sitting on their bike and generally are one of the most lean athletes so low weight. When we look at the elite of the elite, Tour de France contestants, then we don’t see the types of fractures (clavicle, wrist, hand, femure) represented by the location where low BMD is found (femoral neck, total hip, lumbar spine).
“Prevalence and Epidemiology of Injuries Among Elite Cyclists in the Tour de France” https://pubmed.ncbi.nlm.nih.gov/30202769/ “A Systematic Review of Bone Health in Cyclists” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC3230645/
These guys crash at high speeds, off cliffs, against walls etc.. Perhaps we think we understand bone health but do we really? I don’t pretend that I do but at least allow me to challenge the answers we readily give ourselves which is what science expects, question everything.
Understanding bone health
Most people do not think about bones as a dynamic thing but constant remodeling is taking place. Remodeling is taken care of by osteoclasts which break down old and damaged bone while new bone is formed by osteoblasts. A proper balance needs to be maintained between both to support healthy bone and flexible adaptation towards increasing resistance to higher forces such as from resistance exercise and stronger muscle.
Remodeling itself may need to be flexible, increasing when needed and reducing when not required as much.
In studies we find tartrate‑resistant acid phosphatase (TRAP) and collagen degradation via C-terminal telopeptide (CTX) used as a marker of bone resorption while alkaline phosphatase (ALP) and procollagen 1 N-terminal propeptide (P1NP) as a marker of bone formation.

“Disorders of Bone Remodeling” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC3571087/
Often we can look at studies that investigated and found causes of increased fractures such as the next one looking at Type 2 Diabetes (T2D). Due to lower levels of osteocalcin (vitamin K and D deficiency) and bone remodeling, patients have normal BMD but increased risk of fracture. They specifically point out the bad damaged structure rather than BMD as a cause of the higher risk.
According to the article, osteoblasts/osteocytes are impacted in viability and reduces dendrite connectivity through high reactive oxygen species (ROS) when metabolizing glucose. They need a high anti-oxidant defense which is brought up by increased fat metabolism through glutathione.
The following chart is complex but their argument is that decreased bone health is driven by hyperinsulinemia. A KD keeps your insulin very low. One of the results of a higher reliance on carbs is that there are more advanced glycation end products (AGEs) formed. They end up creating cross-links between the collagen, just like the CTX, making the bones more stiff.
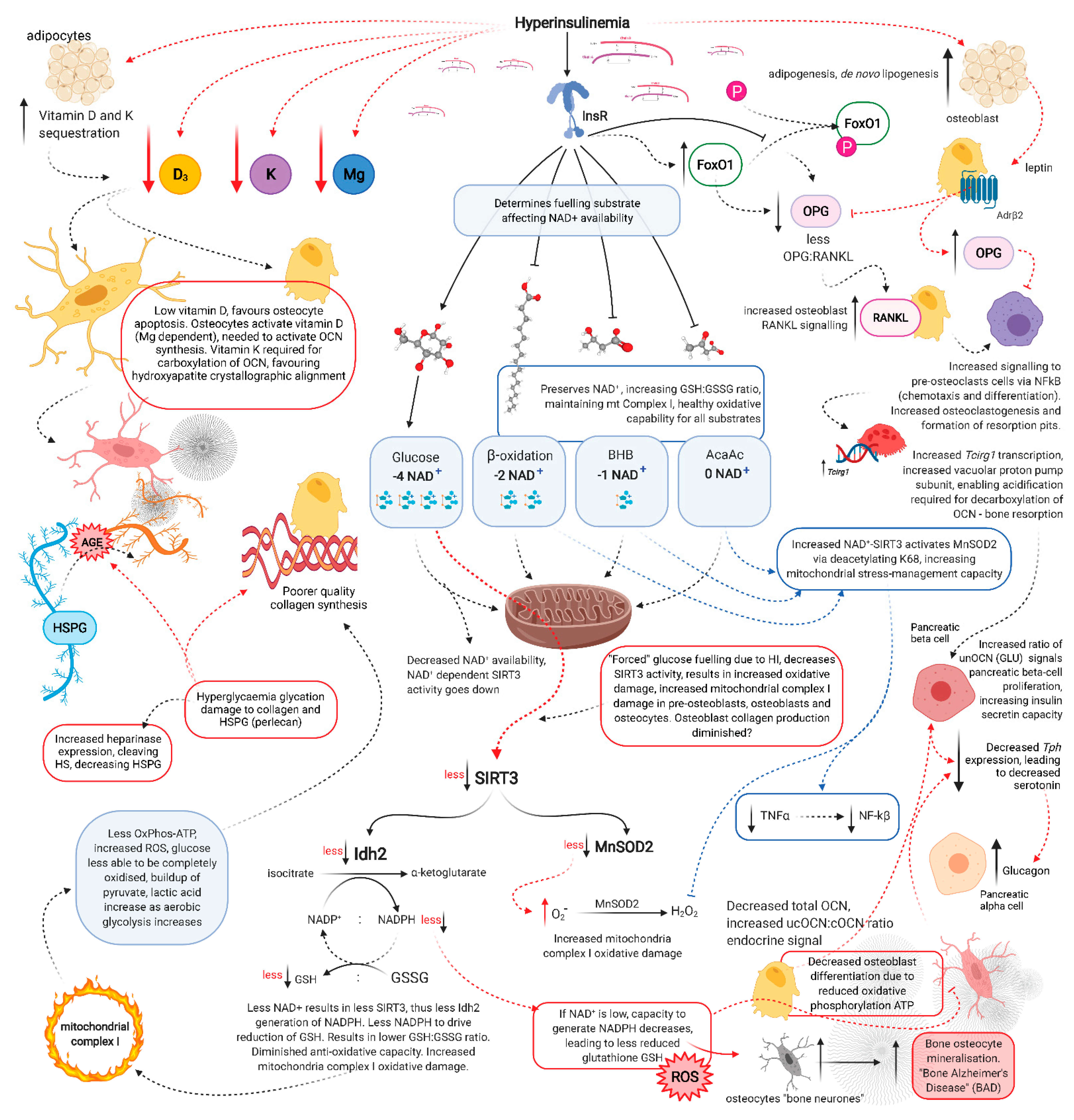
“Rethinking Fragility Fractures in Type 2 Diabetes: The Link between Hyperinsulinaemia and Osteofragilitas” https://www.mdpi.com/2227-9059/9/9/1165
Collagen in the bone is enzymatically cross-linked with each other to provide stiffness. This cross-linking under normal conditions is done by dihydroxylysinonorleucine (DHLNL), hydroxylysinonorleucine (HLNL) and lysinonorleucine (LNL) which are considered the immature links. These substances are easier extracted yet with a lower yield from osteoporotic patients. Over time they further evolve towards mature cross-links pyridinoline (PYD) and deoxypyridinoline (DPD).
The second paper below indicates that especially the immature cross-links are reduced when in competition with AGEs.
Correlations between each of the lysine-derived AGEs (i.e. CML, CEL and pentosidine), and the enzymatic cross-links were analyzed because these AGEs possibly compete with enzymatic crosslinks for formation sites36. The amounts of DHLNL, HLNL, and LNL were negatively correlated with CML, CEL and pentosidine, whereas no such correlation was observed for PYD and DPD (Table 5).
“Reduced concentration of collagen reducible cross links in human trabecular bone with respect to age and osteoporosis” https://pubmed.ncbi.nlm.nih.gov/8922646/ “Mass spectrometric quantitation of AGEs and enzymatic crosslinks in human cancellous bone” https://www.nature.com/articles/s41598-020-75923-8
A further look at T2D confirms the same story. AGEs replace the enzymatic cross-links, increased osteoclast (breaking down) activity and reduction in osteoblast (building up) activity.
The aggregation of AGEs causes non-enzymatic cross-linking of collagen, disrupting the adhesion of osteoblasts to the extracellular matrix and resulting in bone fragility [16] (Fig. 3). These alterations of extracellular matrix also reduce alkaline phosphatase (ALP) activity in mature osteoblasts, affecting bone mineralization [16]. The receptor for AGEs (RAGE) is expressed in human bone cells and its stimulation drives the activation of nuclear factor kappa-B (NF-kB) in osteoclasts, increasing the production of cytokines and reactive oxygen species (ROS) [17]. High proinflammatory cytokine and ROS levels trigger osteoclastogenesis and stop osteoblast differentiation [18, 19].
“Diabetes and Bone Fragility” https://link.springer.com/article/10.1007/s13300-020-00964-1
We can start to doubt if BMD and BMC are good markers of bone health. Bone health lays within the structure but that is not something you can easily measure. DEXA scans give you BMD and BMC but nothing on the integrity.
In line with the effect seen in T2D, we also see how sugar sweetened beverages (SSB) have an inverse association with bone mineral density (BMD).
“Sugar-sweetened beverage consumption and bone health: a systematic review and meta-analysis” https://nutritionj.biomedcentral.com/articles/10.1186/s12937-021-00698-1
To me, this starts to show that BMD and BMC are not quality markers. Looking at a few more studies we find a roughly 50% division for fractures in older adults above and below the WHO determined level for osteoporosis. That makes fracture prediction based on BMD basically a flip-of-a-coin.
“Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study” https://pubmed.ncbi.nlm.nih.gov/14751578/ – “Identification of osteopenic women at high risk of fracture: the OFELY study” https://pubmed.ncbi.nlm.nih.gov/16160738/
Perhaps the combination of these factors, stiffness and lower BMD is something to worry about than either alone?
CTX
CTX exists in different forms. The alpha version, left side on the image below, shows declining levels as we age. Generally everything declines as we age, all for the worse.

“The contribution of collagen crosslinks to bone strength” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC3868729/
Is it possible that we see a decline in CTX because AGEs are replacing them and cannot be broken down so easily?
Vitamin K2
Deficiency in vitamin K2 (vK2) is a factor that could also lead to poor bone health. One of the vK2 effects noted in osteoclast is the inhibition of NF-kB. Too much osteoclast activity and you get weaker bones.
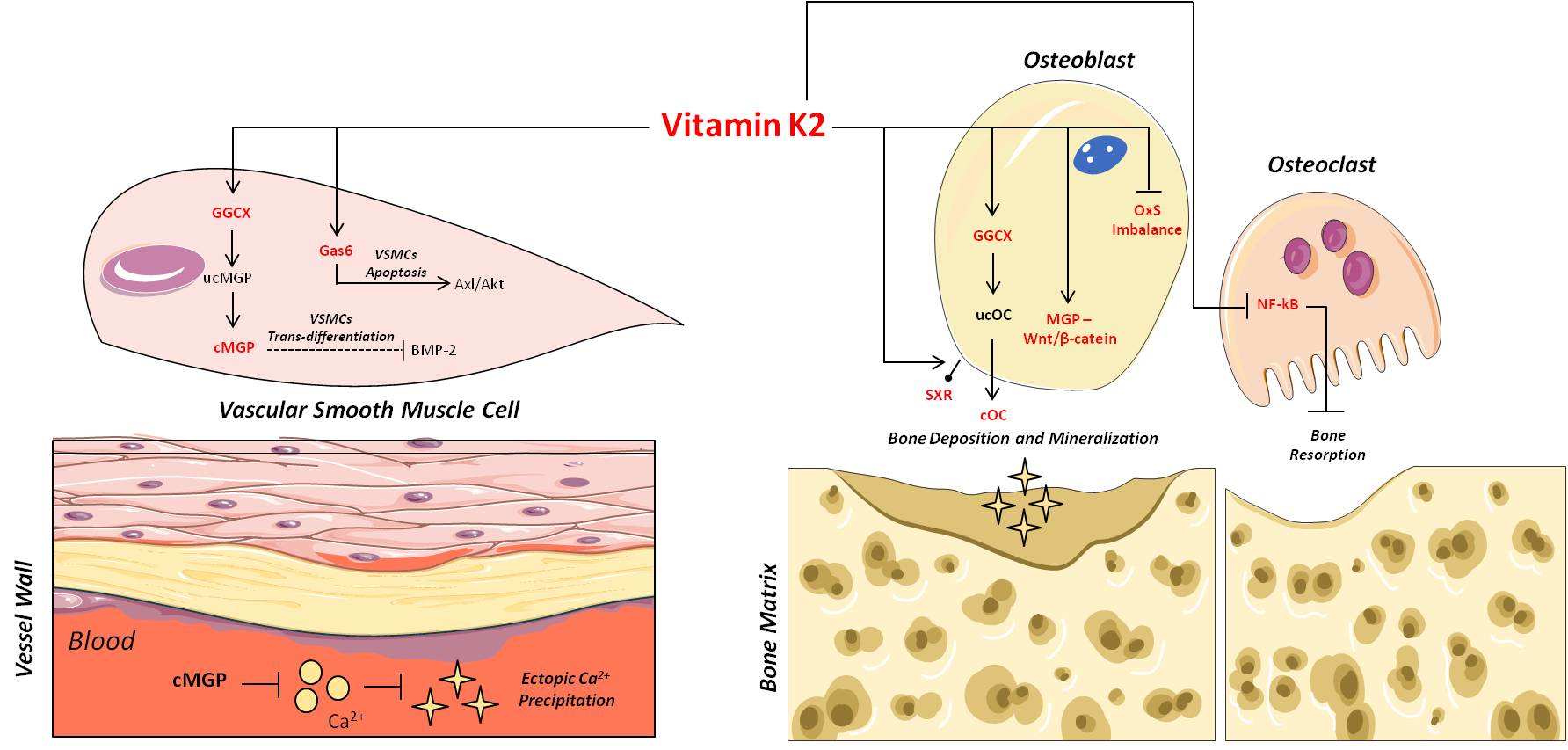
“The Dual Role of Vitamin K2 in “Bone-Vascular Crosstalk”: Opposite Effects on Bone Loss and Vascular Calcification” https://www.mdpi.com/2072-6643/13/4/1222
Vitamin D
Vitamin D has an important role in bone formation. The active form of vitamin D is calcitriol (1,25-dihydroxycholecalciferol). Calcitriol is beneficial to bone formation by inhibiting the osteoclasts and promoting the osteoblast activity.
“Association of Anabolic Effect of Calcitriol with Osteoclast-Derived Wnt 10b Secretion” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC6164019/
Under chronic high fructose intake the levels are reduced.
“Chronic High Fructose Intake Reduces Serum 1,25 (OH)2D3 Levels in Calcium-Sufficient Rodents” https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0093611
Fatty acids
Capric acid also reduces osteoclast activity. But again, it is the balance between osteoclast and osteoblast activity that generates healthy bones.
“A medium-chain fatty acid, capric acid, inhibits RANKL-induced osteoclast differentiation via the suppression of NF-κB signaling and blocks cytoskeletal organization and survival in mature osteoclasts” https://pubmed.ncbi.nlm.nih.gov/25134536/
Different fatty acids have different effects. Here we see octanoic acid and decanoic acid analyzed. Primarily octanoic acid showed a reduction in ALP and increase in TRAP.
“Octanoic acid a major component of widely consumed medium-chain triglyceride ketogenic diet is detrimental to bone” https://www.nature.com/articles/s41598-021-86468-9
Thyroid
In a group of familial longevity they found lower bone turnover markers. Increase in TSH was followed by increase in CTX and P1NP so breakdown and buildup respectively.
“Familial longevity is associated with lower baseline bone turnover but not differences in bone turnover in response to rhTSH.” https://pubmed.ncbi.nlm.nih.gov/34491903
Acidity
One other acid, induced by diet is uric acid. Fructose intake results directly in increased uric acid. Sugar and high fructose corn syrup are major sources of fructose, both via solid and liquid intake. These are highly avoided on a KD.
“Recent advances in fructose intake and risk of hyperuricemia” https://www.sciencedirect.com/science/article/pii/S0753332220309884
Fructose not only causes increased uric acid, it also impairs calcium absorption via the gut.
“Dietary Fructose Inhibits Intestinal Calcium Absorption and Induces Vitamin D Insufficiency in CKD” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2834550/
This is very important because calcium is not only used for bone formation but also for metabolism. With a reduction from the diet, the bones have to give up more calcium to fulfil the needs in the metabolic processes.
Protein
It is so important that it deserves its own chapter. The impact of low dietary protein is often a cause for the noted reduction in bone health and growth stunting in children.
Animal protein stimulates growth more than plant-based protein in children.
“Dietary Intake of Protein in Early Childhood Is Associated with Growth Trajectories between 1 and 9 Years of Age” https://academic.oup.com/jn/article/146/11/2361/4630467
dietary protein is a key nutrient for bone health across the life span and therefore has a function in the prevention of osteoporosis.9 Protein makes up roughly 50% of the volume of bone and about one-third of its mass.10
“Optimizing Dietary Protein for Lifelong Bone Health” https://journals.lww.com/nutritiontodayonline/fulltext/2019/05000/optimizing_dietary_protein_for_lifelong_bone.5.aspx
It should be no surprise that insufficient protein is detrimental for bone formation.
“Protein intake and bone growth” https://pubmed.ncbi.nlm.nih.gov/11897891/
In the elderly population, if anything, we see a reduction in hip fracture with increasing protein. I’m not so happy with these studies. Non-RCT studies as possible positive effects can be impaired by negative confounders such as high glucose and fructose intake.
“Protein intake and risk of hip fractures in postmenopausal women and men age 50 and older” https://link.springer.com/article/10.1007%2Fs00198-016-3898-7 – “Does dietary protein reduce hip fracture risk in elders? The Framingham osteoporosis study” https://link.springer.com/article/10.1007%2Fs00198-010-1179-4 – “Risk Factors for Hip Fracture in Older Men: The Osteoporotic Fractures in Men Study (MrOS)” https://asbmr.onlinelibrary.wiley.com/doi/10.1002/jbmr.2836 – “The Association Between Protein Intake by Source and Osteoporotic Fracture in Older Men: A Prospective Cohort Study” https://asbmr.onlinelibrary.wiley.com/doi/10.1002/jbmr.3058
In the following study we see that particularly a vegan diet is associated with increased fracture. A hazard ratio of 2.31 starts to be meaningful. This is of course just association but perhaps the info further down can help to clarify potential reasons.
“Vegetarian and vegan diets and risks of total and site-specific fractures: results from the prospective EPIC-Oxford study” https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-020-01815-3
In a healthy population, increased dietary protein resulted in increased urinary calcium excretion but this was paralleled with an increase in calcium absorption.
“Dietary protein, calcium metabolism, and skeletal homeostasis revisited” https://academic.oup.com/ajcn/article/78/3/584S/4690000?login=true
Looking again at older adults, animal protein vs plant protein vs total protein we see that protein intake is important and animal protein gives a significant increase in BMD over plant protein.

“Protein intake and bone mineral density: Cross-sectional relationship and longitudinal effects in older adults” https://onlinelibrary.wiley.com/doi/10.1002/jcsm.13111
Fractures
Racing bikes are made of a carbon frame. These are very stiff and very strong but only when the force is applied in the right direction. Parallel to the tube, not sideways. Sideways they don’t bend, they snap like a dry twig. Could the same be the case for our bones?
AGEs
One potential contributor to decreased bone health is pentosidine which is an AGE. We saw before that AGEs form bad quality collagen links, creating stiffer bones.
Pentosidine content in bone tends to increase in an age-dependent manner, and different diseases can accelerate the accumulation of pentosidine. Studies in animal models of type 2 diabetes, type 1 diabetes, low and high turnover chronic kidney disease, and postmenopausal osteoporosis have shown elevated levels of bone pentosidine and altered amounts of enzymatic cross-links (lysyl oxidase [LOX]-dependent cross-links). As these diseases are also associated with higher fracture risk, the hypothesis is that pentosidine contributes to fracture risk.
“Pentosidine as a Biomarker for Poor Bone Quality and Elevated Fracture Risk” https://link.springer.com/referenceworkentry/10.1007%2F978-94-007-7693-7_32
Since glycation is often reported as glucose binding with protein, it is often forgotten that fructose (fructation) has an even bigger effect, up to 10-fold higher!
“Nonenzymatic glycation of bovine serum albumin by fructose (fructation). Comparison with the Maillard reaction initiated by glucose” https://pubmed.ncbi.nlm.nih.gov/2537288/
Not only within the body but also via our diet do we ingest AGEs. This Japanese study looked at common food and drinks. At the bottom end we see milk, coffee and tea but the top shows sugar and fructose containing drinks for the most part.
“Assessment of the Concentrations of Various Advanced Glycation End-Products in Beverages and Foods That Are Commonly Consumed in Japan” https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0118652
Such dietary AGEs and endogenously produced ones depend on good filtration capability of the kidneys, which are impaired under metabolic syndrome.
“Studies on Absorption and Elimination of Dietary Maillard Reaction Products” https://nyaspubs.onlinelibrary.wiley.com/doi/abs/10.1196/annals.1333.054
To no surprise, people who suffer from chronic kidney disease have elevated serum AGEs and this is reflected in their bones with increased fracture risk.
Pentosidine was remarkably increased in dialysis patients and inversely correlated with bone-formation rate/bone volume and mineral apposition rate. This study suggests that AGE collagen cross-links strongly associate with disorders of bone metabolism in dialysis patients.
“Nonenzymatic cross-linking pentosidine increase in bone collagen and are associated with disorders of bone mineralization in dialysis patients” https://pubmed.ncbi.nlm.nih.gov/21499867/
The enzymatic cross-links is what we want, not pentosidine. By increasing the enzymatic ones and removing pentosidine, we see in the following study an increase in strength. Both calcium content and these enzymatic cross-links were each independently responsible for increased strength. Also in this study they reaffirm that the cross-links determined stiffness.
“Changes in the contents of enzymatic immature, mature, and non-enzymatic senescent cross-links of collagen after once-weekly treatment with human parathyroid hormone (1-34) for 18 months contribute to improvement of bone strength in ovariectomized monkeys” https://pubmed.ncbi.nlm.nih.gov/20959962/
Impact on a ketogenic diet
A KD avoids carbs and fructose in the diet especially from sugar and high-fructose corn syrup (HFCS) and sugar containing beverages, even ‘natural’ fruit drinks which are also high in carbs.
So a reduction in glucose which forms AGEs, a normal or increased calcium uptake due to lower fructose, lower uric acid due to low fructose and sufficient protein.
The diet generally elevates vitamine D and K2 sources and allows stored vitamine D to be released from adipose as weight is lost.
Not only vK2 can suppress NF-kB but also a ketogenic diet.
“Ketogenic diet attenuates oxidative stress and inflammation after spinal cord injury by activating Nrf2 and suppressing the NF-κB signaling pathways” https://pubmed.ncbi.nlm.nih.gov/29894768/
Following an 8-week KD, women on resistance training had a small significant improvement in BMD compared to the normal diet (0.02 versus 0.00 g/cm2).
“Effects of a low-carbohydrate ketogenic diet on health parameters in resistance-trained women” https://link.springer.com/article/10.1007%2Fs00421-021-04707-3
After 12 weeks on a KD, there were no differences found in BMD.
“Keto-adaptation enhances exercise performance and body composition responses to training in endurance athletes” https://www.metabolismjournal.com/article/S0026-0495(17)30298-6/fulltext
A thorough review of bone remodeling and ketogenic diet has been done before but they somewhat left out the impact of dietary protein. A must-read though to get a better understanding in general. It covers a lot of murine studies. Important is that a KD for these animals usually involves highly restricted protein intake.
“Energy Metabolism and Ketogenic Diets: What about the Skeletal Health? A Narrative Review and a Prospective Vision for Planning Clinical Trials on this Issue” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC7796307/
Following up epileptic children who followed a modified Atkins diet (MAD), less restrictive in protein, they found no impact on bone health. Normal bone mass and growth.
“Prospective study of growth and bone mass in Swedish children treated with the modified Atkins diet” https://pubmed.ncbi.nlm.nih.gov/31085021/
Acidity
A KD is typical because it raises the production of beta-hydroxybutyrate (BHB) which is an acid. You could quickly jump to conclusion that this acid needs to be neutralized by binding to calcium leading to calcium deprivation impacting bone formation.
What we do notice is that the pH is maintained within the required range (7.35 – 7.45). A KD reduces the production of CO2 which is also an acid.
I don’t have data to support the following claim but I think it makes sense. When the diet can supply sufficient calcium then it is likely that the balance is kept to deal with acidity so that the bones are not impacted.
The dietary sources on a ketogenic diet are sufficiently high in calcium and the level of protein intake should support calcium requirements.
Protein
Some people claim that protein intake is responsible for acidity. Proteins are made up of amino acids thus indeed also acidic. But a thorough study measuring urine pH, acid excretion and calcium excretion found no relationship with fractures in a long follow-up study of 5 years, including no change in BMD.
“Low urine pH and acid excretion do not predict bone fractures or the loss of bone mineral density: a prospective cohort study” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2890599/
It even seems that protein help to clear uric acid!
“The uric acid lowering effect of protein-rich diets. Behavior of human uric acid metabolism under reducing diet forms with varied protein content” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC2890599/
Studies in mice and rats often involve heavy restriction of protein in the diet. Could that influence the results? This is definitely a confounder.
AGEs
This study concluded a low carbohydrate diet reduced renal AGE formation.
“Low-Carbohydrate Diet Inhibits Different Advanced Glycation End Products in Kidney Depending on Lipid Composition but Causes Adverse Morphological Changes in a Non-Obese Model Mice” https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC6893679/
Summary
Bone Mineral Density is not an indication of bone health. Bone health and remodeling can be impacted by many factors.
- Increased force requires more remodeling to create a higher density.
- When switching from a diet that is detrimental for bone health towards one that is good for bone health may be marked by a temporal increase in breakdown markers, especially CTX.
- Protein in the diet needs to be sufficient. Restricting it too severe such as in animal studies and often in children treated for epilepsy on a KD, will lead to reduced bone density.
- Something we see in astronauts is that they lose 1% to 2% of BMD every month. Weight loss reduces the strength requirements so we can expect a little reduction in BMD noticeable via higher breakdown activity.
- Adequate nutritional status of vK2 and calcitriol are important bone mass forming agonists and together with a KD reduce bone breakdown activity.
“What happens to bones in space?” https://www.asc-csa.gc.ca/eng/astronauts/space-medicine/bones.asp
So when studies report a negative effect on BMD then we need to look at all these effects and evaluate whether we are looking at a desired effect or an impaired situation.
The only objective markers for bone health can be found on incidences of fracture rates.
As long as we don’t see an increase in weight lifters and endurance athletes, who have a higher dependency on quality bones, more easily exposed to bone breaking activities, then all we have is association of incorrectly understood markers of bone dynamics.
Similarly, the elderly population is also at increased risk. If we see no difference on a KD then I would consider it safe and a non-issue.
Attacks
Now that we have a little better understanding, returning back to the first paper. The next picture summarizes their conclusions.
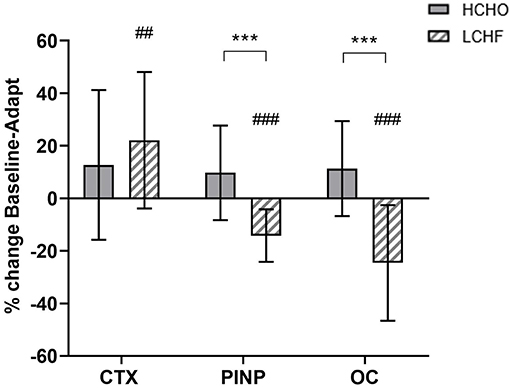
CTX is related to collagen while osteoclasts are directly active in the breakdown process. Yet osteoclasts see a drastic reduction. In the diseased states such as CKD and T2D we saw increased osteoclast activity. We saw higher CTX activity in the young versus old population.
So the KD seems to resemble the young and healthy bone dynamics rather than a detrimental one. A stark contradiction in conclusion while the data remains the same.
For CTX we don’t really see any meaningful difference except right after exercise.

Rather than concluding impaired bone health, I would rather raise questions on the understanding of CTX. Especially when CTX and osteoclasts should be in agreement but here are opposite to each other.
Wikipedia is clear about this:
The CTX test measures for the presence and concentration of a crosslink peptide sequence of type I collagen, found, among other tissues, in bone. This specific peptide sequence relates to bone turnover because it is the portion that is cleaved by osteoclasts during bone resorption, and its serum levels are therefore proportional to osteoclastic activity at the time the blood sample is drawn.
source: https://en.wikipedia.org/wiki/C-terminal_telopeptide
P1NP may be in line with reduced osteoclast assuming you don’t need as much buildup when the breakdown is reduced.
“A Short-Term Ketogenic Diet Impairs Markers of Bone Health in Response to Exercise” https://www.frontiersin.org/articles/10.3389/fendo.2019.00880/full?utm_source=F-NTF&utm_medium=EMLX&utm_campaign=PRD_FEOPS_20170000_ARTICLE
Furthermore, the study was done short-term (3-3.5 weeks) while we’ve seen a study of 12 weeks showing no negative effect when just looking at BMD.
In other words, shortsighted conclusions .
Food for thought but fear of impaired bone health on a ketogenic diet is not something I’m concerned about. Until further better quality studies paint a different picture.
Update 2023-03-16:
BHB is shown to extend life of the chondrocytes. Referencing wikipedia, these are the only cells found in cartilage and they maintain the cartilage matrix, producing collagen and proteoglycans.
“β-Hydroxybutyrate alleviates cartilage senescence through hnRNP A1-mediated up-regulation of PTEN” https://www.sciencedirect.com/science/article/pii/S053155652300061X
—- T H E – E N D —-
Leave a comment